If you want to ease into an exercise option that is good for all ages, then consider yoga Many people turn to
MoreIt’s important to stay alert for skin cancer, but it’s important to acknowledge that other ‘safe’ skin conditions such as skin tags,
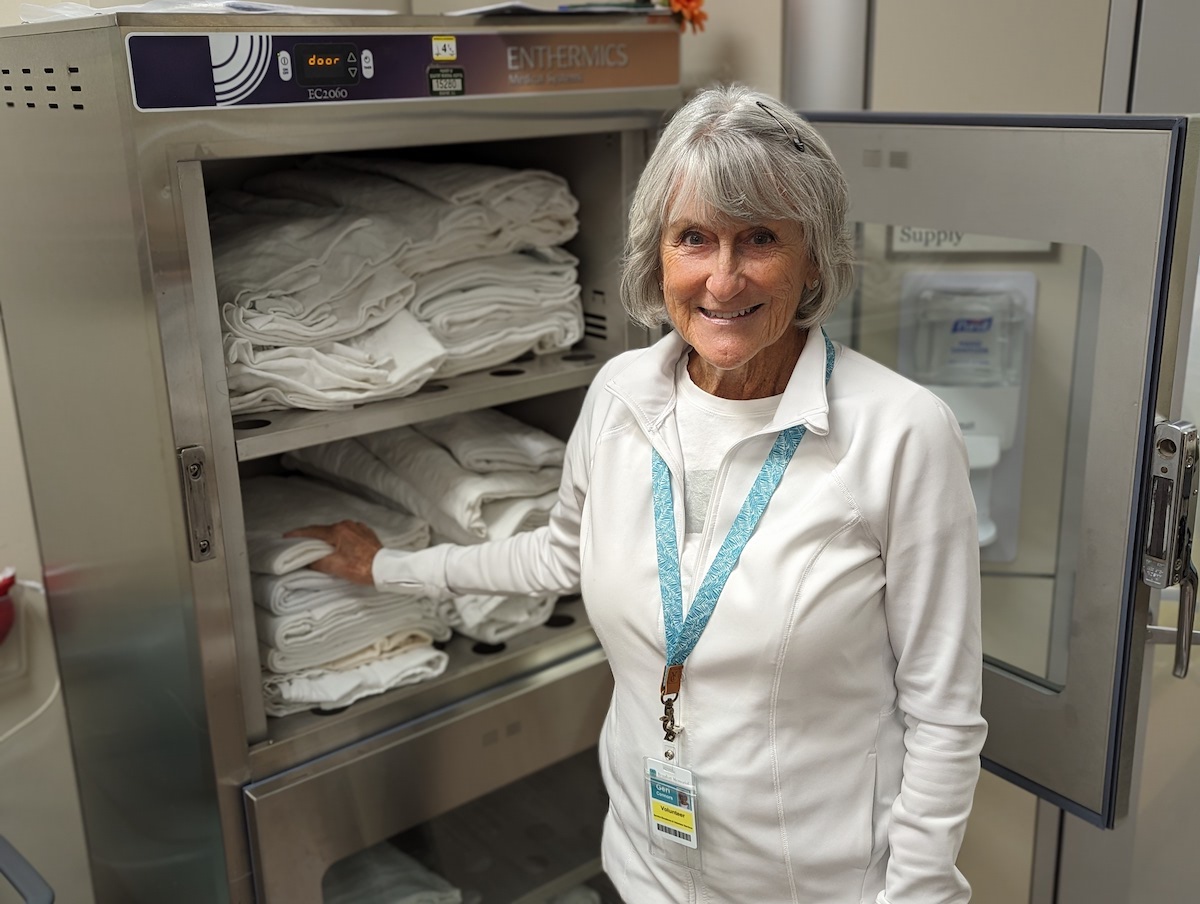
MoreBy Courtney McDermott Editor’s note: This week (April 21-27) is National Volunteer Week, an opportunity to recognize the impact of volunteer service and the
MorePeople have anecdotally claimed that the timing of a meal may affect metabolism, but there isn’t much solid evidence in support. To
MoreYou’re going about your day, when all of a sudden, you feel a throbbing or pounding pain in your head. Great, you’ve
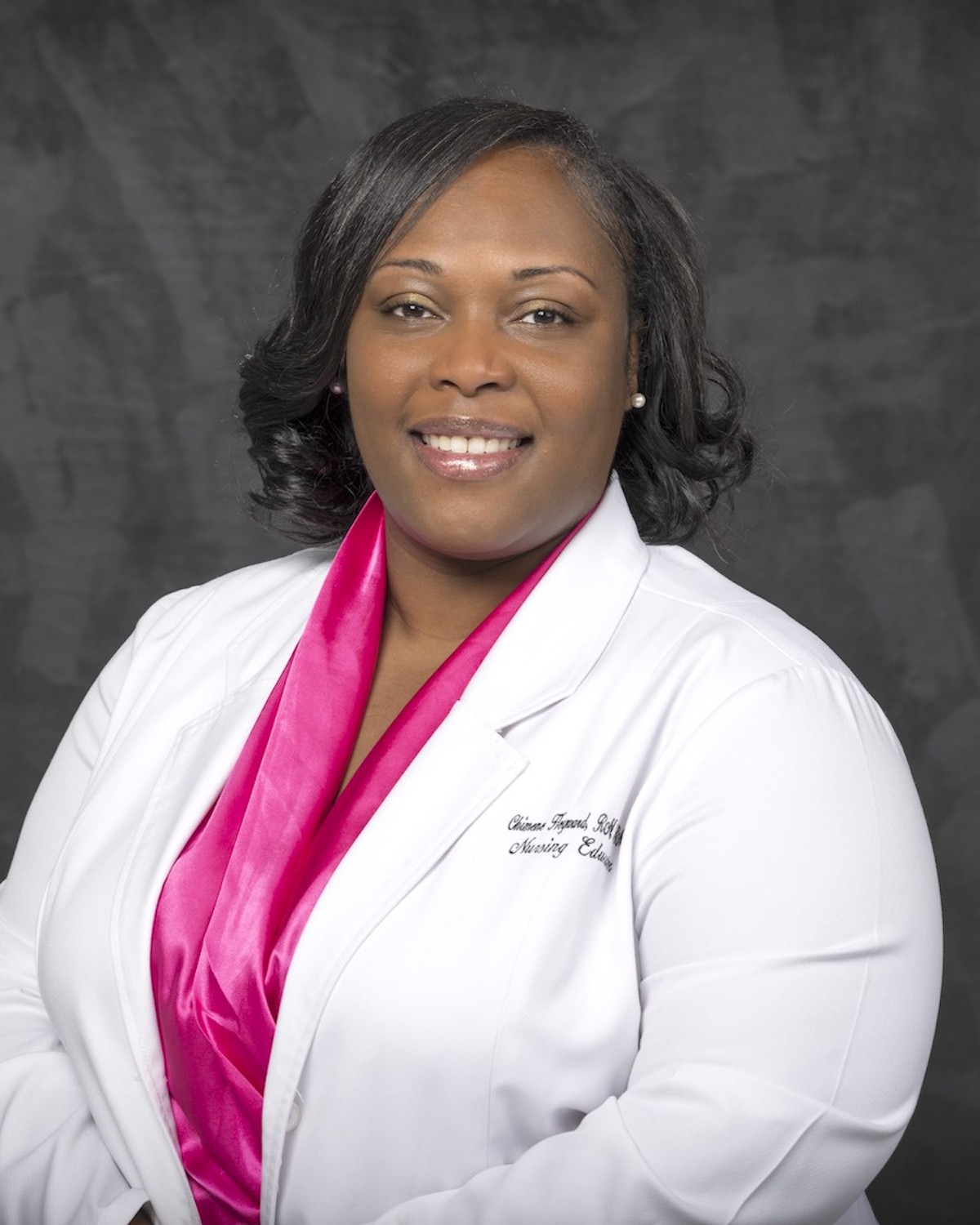
MoreChimene Heyward, MSN, RN, has joined the Beaufort Memorial Breast Health Center in Okatie and Beaufort as a breast care nurse navigator. At the centers, Heyward guides breast cancer patients from diagnosis
More